Last Updated: 19 September 2022
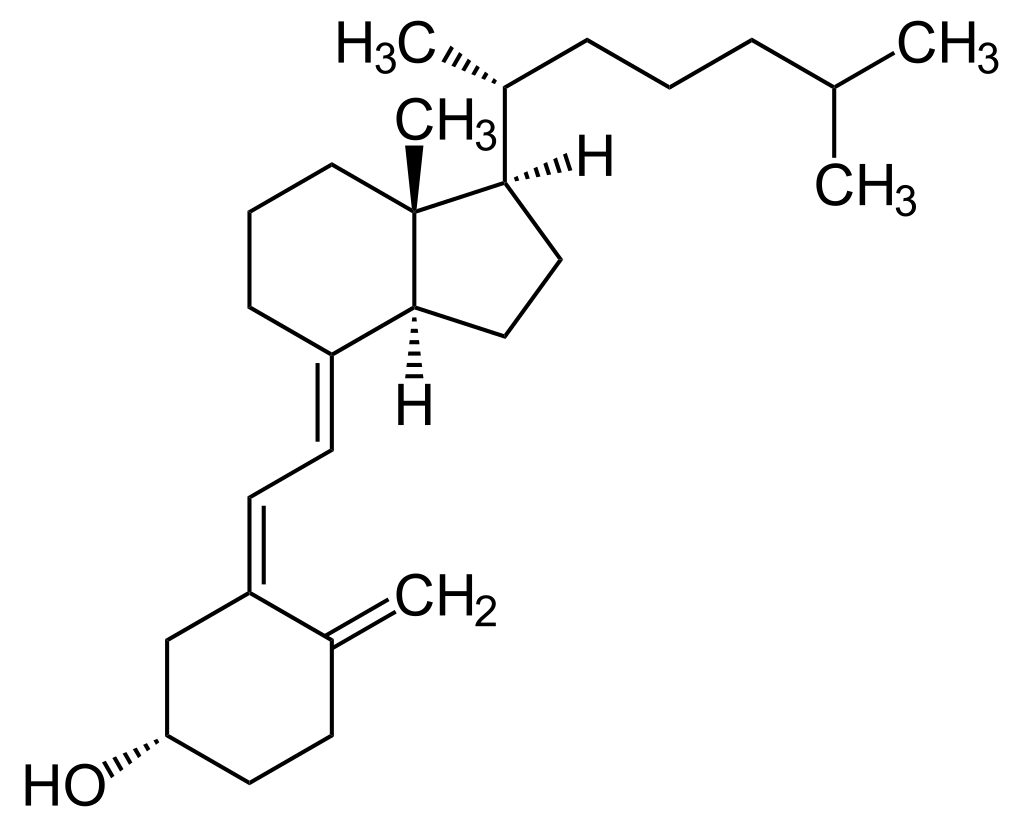
Figure 1. The chemical structure of cholecalciferol (or Vitamin D3).
Vitamin D is a group of fat soluble compound responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and many other biological effects. In humans, the most important compounds in this group are vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol, a provitamin D). In the human body, Vitamin D is primarily synthesised as cholecalciferol (Vitamin D3) in the lower layers of epidermis of the skin through a chemical reaction that is dependent on sun exposure, specifically ultraviolet B radiation. Vitamin D2 is synthesised in some plants and funghi.
Vitamin D produced from skin synthesis or obtained from diet are biologically inactive. In its original form, Vitamin D is considered a hormone. It must be activated by two protein enzyme hydroxylation steps, the first in the liver and the second in the kidneys, in order to transform into its biologically active form. Cholecalciferol and ergocalciferol are converted in the liver to calcifediol (25-hydroxycholecalciferol) and 25-hydroxyergocalciferol respectively. Then, in the kidneys and some immune system cells, calcifediol is further hydroxylated to form calcitriol, the biologically active form of Vitamin D.
Calcitriol circulates as a hormone in the blood, playing a major role in regulating the concentration of calcium and phosphate in the body, and promoting the healthy growth and remodelling of bone. Calcitriol also has other health effects, including cell growth, neuromuscular and immune functions, and reduction of inflammation. Many of the body’s organs and tissues have receptors for Vitamin D, which suggest important roles beyond bone health.
There are very few food sources that are naturally rich in Vitamin D3. The best food sources are fatty fish and fish liver oils. Examples include:
As a dietary supplement, Vitamin D is taken mainly to treat Vitamin D deficiency. Worldwide, an estimated 1 billion people have inadequate levels of Vitamin D in their blood, and deficiencies can be found in all ethnicities and age groups. Vitamin D deficiency may occur from a lack in the diet, poor absorption, or having a metabolic need for higher amounts. People who cannot tolerate or do not eat milk, eggs, and fish, such as those with a lactose intolerance or who follow a vegan diet, may also be at higher risk for Vitamin D deficiency. When left untreated, prolonged Vitamin D deficiency may result in diseases like rickets and osteomalacia (weak and soft bones). Vitamin D is also commonly promoted to help reduce the risk of cancer, heart diseases, type 2 diabetes, and to boost the immune system.
The Recommended Dietary Allowance for adults 19 years and older is 15mcg daily for men and women, and for adults more than 70 years it is 20mcg daily. The Tolerable Upper Intake Level is the maximum daily intake unlikely to cause harmful effects on health, and this level for Vitamin D for adults and children ages 9+ is 100mcg.
While it is unlikely to experience Vitamin D toxicity via one's diet or from sun exposure, toxicity can occur from consuming excessive Vitamin D supplements. Symptoms of Vitamin D toxicity include anorexia, weight loss, irregular heartbeat, and hardening of blood vessels and tissues leading to heart and kidney damage.
Vitamin D, more specifically calcitriol, is listed in the World Health Organization's List of Essential Medicines.
Sources and Citations:
* Please be advised: always seek medical consultation if you require medical help or attention. The contents of this Codex are for educational purposes and are not intended to offer personal medical advice.